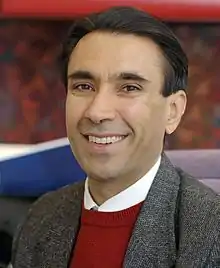
Sanjeev Arora (physician)
Sanjeev Arora, MD, MACP, FACG (born September 1956), an Indian-American physician, is the Founder and Director of Project ECHO (Extension for Community Healthcare Outcomes),[1] a telementoring model for quickly scaling up health expertise in local communities.
Sanjeev Arora | |
|---|---|
 | |
| Born | September 1956 (age 65) |
| Citizenship | United States |
| Alma mater | Armed Forces Medical College, Maharahah College |
| Scientific career | |
| Fields | Medicine, Telehealth, Telemedicine |
| Institutions | University of New Mexico School of Medicine |
Dr. Arora is also a Distinguished Professor of Medicine, Director of the Office of Clinical Affairs, and Executive Vice Chair for the Department of Internal Medicine at the University of New Mexico Health Sciences Center (UNMHSC) in Albuquerque. Dr. Arora developed and implemented the Hepatitis C Disease Management Program at UNMHSC.
Education
Dr. Arora received a premedical degree from Maharajah College in Jaipur, India, followed by his medical degree at the Armed Forces Medical College, in Pune, India, and an internship at Army Hospital, Delhi. He completed several residencies, first in medicine at Safdarjung Hospital in New Delhi, then for surgery at Maimonides Medical Center in Brooklyn, NY, returning to medicine at the Sisters of Charity Hospital, State University of New York in Buffalo. He completed his fellowship in gastroenterology at the New England Medical Center in Boston.
Career
Following his studies, Dr. Arora began his career in academia in 1987, first as an Assistant Professor of Medicine at Tufts University. He then moved to the University of New Mexico in 1993, where he served in various positions, including Section Chief of Gastroenterology and Associate Professor, Chief of Medical Staff, Director at the Office of Clinical Affairs, Executive Vice-Chair of the Department of Internal Medicine, and Distinguished Professor of Medicine.
While working as a liver disease specialist at UNMHSC, Dr. Arora became frustrated that he could treat only a fraction of the more than 28,000 New Mexicans with hepatitis C. His wait list to see patients was eight months, and people were dying. In response, he created Project ECHO to share his expertise with primary care providers in rural communities. The new ECHO program resulted in 21 new centers of excellence equipped to treat hepatitis C across New Mexico.
Project ECHO
Launched in 2003, Project ECHO is a guided-practice model that uses one-to-many videoconferencing technology and case-based learning to reduce health disparities in underserved and remote areas. The model has a hub-and-spoke structure: Teams of medical specialists and experts at regional, national, and global medical centers (the “hubs”) connect with community-based doctors, nurses, and other health providers (the “spokes”) in weekly virtual clinics that include brief didactics, case presentations, and discussion. In this way, primary care providers become adept in best practices for treating patients in their communities with diseases ranging from hepatitis C and tuberculosis to cancer and HIV.
More than Bibliography Apr 2020.pdf 300 peer-reviewed studies attest to ECHO’s effectiveness,[2] including a landmark 2011 evaluation published in the New England Journal of Medicine.[3]
After starting in New Mexico, Project ECHO quickly spread across the United States and then around the world. As of December 2020, ECHO partners in 40 countries were operating more than 860 ECHO learning networks.
ECHO’s first Africa program launched in Namibia in 2015, to address HIV. As of December 2020, 33 hub partners in 14 African countries operated ECHO programs in areas such as HIV, epi-surveillance, and laboratory strengthening. In 2019, these partners trained more than 50,000 participants.
ECHO India[4] has operated since 2008, starting with various healthcare initiatives and now applying the ECHO model to areas such as education and pollution. In 2019, partners in India trained more than 250,000 participants.
When COVID-19 struck, Project ECHO pivoted its resources to addressing the pandemic. ECHO programs in the United States and internationally shifted focus to address COVID-19. The ECHO Institute partnered with federal government agencies, including the Centers for Disease Control and Prevention and the U.S. Department of Health and Human Services Assistant Secretary for Preparedness and Response, to launch new COVID-19 training programs in the United States and abroad.
The AHRQ ECHO National Nursing Home Network[5] is its latest initiative to combat COVID-19, in partnership with the federal Agency for Healthcare Research and Quality (AHRQ) and the Institute for Healthcare Improvement (IHI). In less than two months, the Network launched 100 training centers to mentor and support staff in 8,000 nursing homes in COVID1-9 infection control and prevention.
In December 2020, ECHO programs launched training units in COVID-19 vaccination.
In 2020, Project ECHO became one of six finalists in the John D. and Catherine T. MacArthur Foundation’s 100&Change competition, a $100 million grant that funds a single proposal that promises real and measurable progress in solving a critical problem.[6]
Policy
In the waning days of 2016, an outgoing Congress and President approved the original version of the ECHO Act,[7] which helped catalyze spread of the ECHO model across the country. In December 2020, as part of the pandemic emergency relief package, Congress passed a new measure that creates a $50 million, five-year program under HHS to award grants for developing, expanding, and evaluating the use of models like ECHO to increase access to health care services and improve the retention of health care providers in underserved communities.
Awards and honors
Brock Prize in Education Innovation Laureate
2021 - Brock Prize in Education Innovation
The Brock Prize in Education Innovation is built upon the belief that the most important thing we do in life is to educate the next generation. The prize rewards ideas proven to enhance education, and which have global impact, universal accessibility and a proven track record.
Zoomtopia Innovation Award: Exceptional Healthcare
2020 - Zoom
Since the start of the pandemic, Project ECHO has used Zoom to deliver critical information and education about COVID-19 to hospitals and healthcare clinics around the globe, providing them the knowledge they need to treat the virus and save lives.
Project ECHO has been leveraging Zoom to reach healthcare workers since 2013.
Lifetime Recipient – Governor's Public Service Award
2019 - Governor of New Mexico
Selected Articles
Arora, S., Thornton, K., Komaromy, M., Kalishman, S., Katzman, J., & Duhigg, D. (2014). Demonopolizing medical knowledge. Academic medicine, 89(1), 30-32.[8]
Arora, Sanjeev, et al. "Outcomes of treatment for hepatitis C virus infection by primary care providers." New England Journal of Medicine 364.23 (2011): 2199-2207.[9]
Arora, Sanjeev, et al. "Partnering urban academic medical centers and rural primary care clinicians to provide complex chronic disease care." Health Affairs 30.6 (2011): 1176-1184.[10]
Arora, Sanjeev, et al. "Expanding access to hepatitis C virus treatment—Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care." Hepatology 52.3 (2010): 1124-1133[11]
Notes
- "Project ECHO". hsc.unm.edu. Retrieved 2021-03-23.
- Bibliography Apr 2020.pdf "Peer-Reviewed Studies" (PDF).
{{cite web}}: Check|url=value (help)CS1 maint: url-status (link) - Arora, Sanjeev; Thornton, Karla; Murata, Glen; Deming, Paulina; Kalishman, Summers; Dion, Denise; Parish, Brooke; Burke, Thomas; Pak, Wesley; Dunkelberg, Jeffrey; Kistin, Martin (2011-06-09). "Outcomes of Treatment for Hepatitis C Virus Infection by Primary Care Providers". New England Journal of Medicine. 364 (23): 2199–2207. doi:10.1056/NEJMoa1009370. ISSN 0028-4793. PMC 3820419. PMID 21631316.
- India, ECHO. "Project ECHO - India". echoindia.in. Retrieved 2021-03-23.
- "Nursing Home Information | Nursing Home COVID-19 Action Network". hsc.unm.edu. Retrieved 2021-03-23.
- "Project ECHO - MacArthur Foundation". MacArthur Foundation. June 24, 2021.
- Hatch, Orrin G. (2016-12-14). "S.2873 - 114th Congress (2015-2016): ECHO Act". www.congress.gov. Retrieved 2021-03-23.
- Arora, Sanjeev; Thornton, Karla; Komaromy, Miriam; Kalishman, Summers; Katzman, Joanna; Duhigg, Daniel (1 January 2014). "Demonopolizing medical knowledge". Acad Med. 89 (1): 30–32. doi:10.1097/ACM.0000000000000051. PMID 24280860.
- Arora, Sanjeev; Thornton, Karla; Murata, Glen; Deming, Paulina; Kalishman, Summers; Dion, Denise; Parish, Brooke; Burke, Thomas; Pak, Wesley; Dunkelberg, Jeffrey; Kistin, Martin; Brown, John; Jenkusky, Steven; Komaromy, Miriam; Qualls, Clifford (9 June 2011). "Outcomes of treatment for hepatitis C virus infection by primary care providers". N. Engl. J. Med. 364 (23): 2199–2207. doi:10.1056/NEJMoa1009370. PMC 3820419. PMID 21631316.
- Arora, Sanjeev; Kalishman, Summers; Dion, Denise; Som, Dara; Thornton, Karla; Bankhurst, Arthur; Boyle, Jeanne; Harkins, Michelle; Moseley, Kathleen; Murata, Glen; Komaramy, Miriam; Katzman, Joanna; Colleran, Kathleen; Deming, Paulina; Yutzy, Sean (1 June 2011). "Partnering urban academic medical centers and rural primary care clinicians to provide complex chronic disease care". Health Aff (Millwood). 30 (6): 1176–1184. doi:10.1377/hlthaff.2011.0278. PMC 3856208. PMID 21596757.
- Arora, Sanjeev; Kalishman, Summers; Thornton, Karla; Dion, Denise; Murata, Glen; Deming, Paulina; Parish, Brooke; Brown, John; Komaromy, Miriam; Colleran, Kathleen; Bankhurst, Arthur; Katzman, Joanna; Harkins, Michelle; Curet, Luis; Cosgrove, Ellen; Pak, Wesley (1 September 2010). "Expanding access to hepatitis C virus treatment--Extension for Community Healthcare Outcomes (ECHO) project: disruptive innovation in specialty care". Hepatology. 52 (3): 1124–1133. doi:10.1002/hep.23802. PMC 3795614. PMID 20607688.